Guided Self-Rehabilitation Lab
SRT | Self-Rehabilitation
Technology
Guided self-rehabilitation lab
SRT | Self-Rehabilitation Technology
Break the cycle of physical inactivity
Ageing population is a challenge for healthcare systems. Collectively, we need to find solutions to develop intensive and diversified care pathways.
- The World Stroke Organisation recommends 3 hours of rehabilitation per day after a stroke.
- According to Barrett et al. (2018), prolonged inactivity periods reach 5.3 hours on weekdays and 6.8 hours during weekends.
These periods maintain deconditioning effects that affect patients’ recovery. Studies show that increasing activity time for patient is an essential factor in the functional recovery and autonomy maintenance.
Daily life of a rehab patient
During weekdays
Rest: 22%
Physical therapy: 7%
During weekends
Sleep: 41%
Rest: 21%
Source : Barret et al . (2018)

Our vision
The Guided Self-rehabilitation Lab
Based on the previous observation, it is therefore essential to involve patients in their rehabilitation. Therapists and relatives should also motivate them to increase the amount of daily activity.
Integrating a guided self-rehabilitation lab into the care pathway helps to reduce inactivity time and makes the patient actor in his or her own rehabilitation.
It consolidates and improves motor recovery, in addition to conventional therapy. Thanks to this innovative approach,risk of physical condition loss and autonomy loss are limited.
The therapists remain essential and guide the patient towards exercises adapted to their recovery stage.
A rich and open space
to make patients actors in their rehabilitation

In autonomy
The patient can come in autonomy alone, with other patients or with their family and caregivers.

Supervised group
The space can also be used for supervised group therapy with multiple patients.
SRT | Self-Rehabilitation Technology
These devices can be used outside of conventional rehabilitation sessions:
- In a self-rehabilitation space
- In supervised group therapy
- The patient focuses on performing and repeating the movement through cognitive and motor activities.
Ultra-intuitive, SRT devices are accessible to both children and the elderly, in a sitting or standing position.
The patient’s actions are transcribed in real time on the screen.
The patient can perform the various activities unimanually or bimanually, alone, with other patients, or with loved ones. Many cognitive-motor activities are already available to keep the patient motivated and involved in their rehabilitation.

It forces us to make simple movements.
I’ll try all the different devices to maximize my chances.”
Claudine, patient
– IRR LNA Romainville (FR)
Set of 3 devices to adapt to all kind of patients,
from less motor impairments to severe

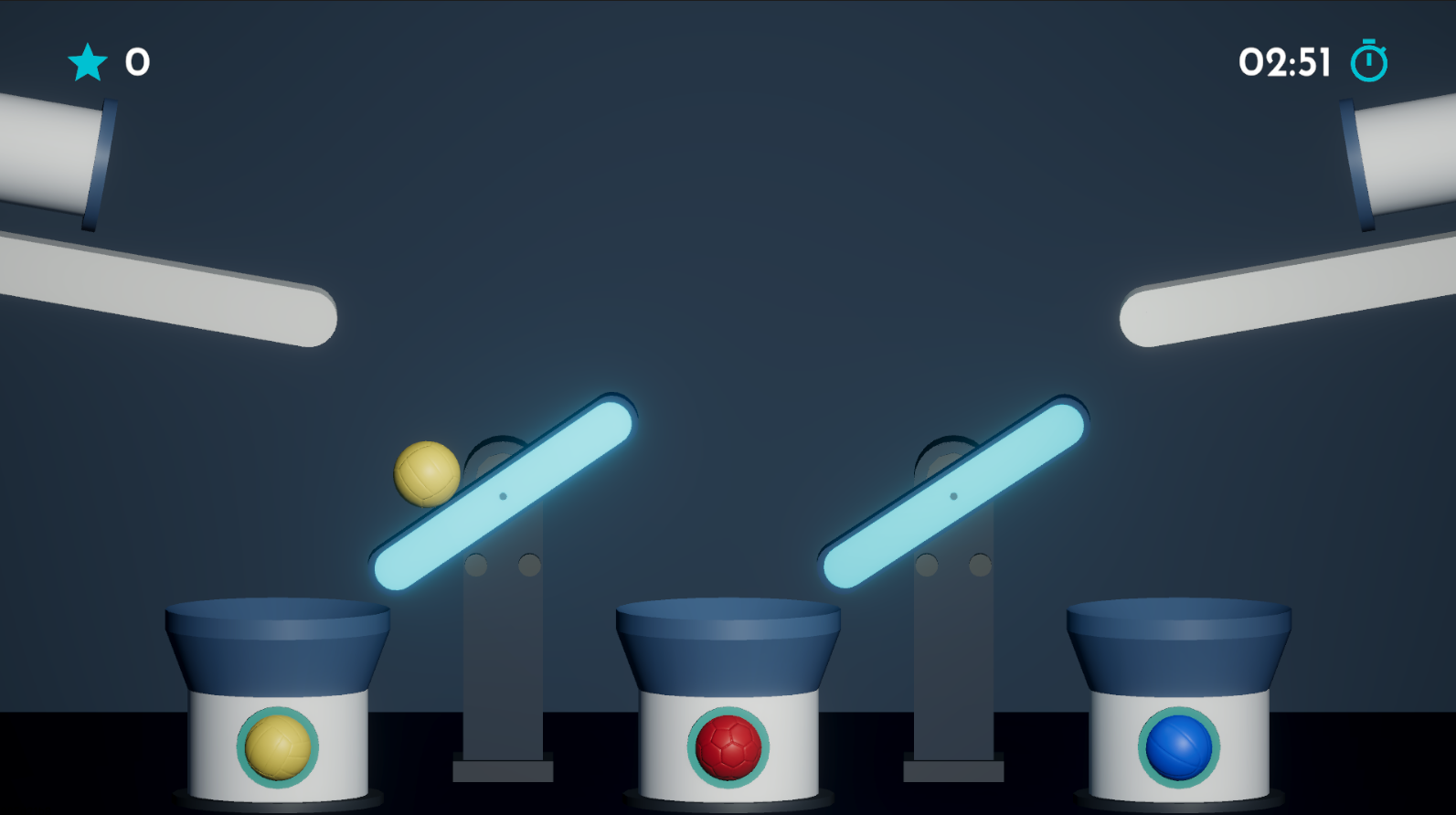
SRT5
- Work on global movement, focusing on elbow and shoulders
- Possible to constraint the use of the pathological hand

SRT2
- Work on bimanual coordination
- Requires less arm elevation
- Intensive training on wrists movements

SRT6
- Accessible for patients with limited proximal movements (shoulders)
- Intensive training on hand and wrist
- Work on attention and multi-sensations (screen + spheres)

Steve, patient
– Rothschild Hospital (FR)
Complementary
technologies
All SRT devices offer common exercises in order to adapt work to patients’ motor recovery, or in order to work on the same activity but in a different way.
Cognitive-motor activities are adapted to each device. Exclusive activities are also developed in order to diversify training possibilities.
By practising in the guided self-rehabilitation lab, patients develop :
- balance in standing position
- double-task, especially on SRT2 and SRT6, with screen and random spheres management
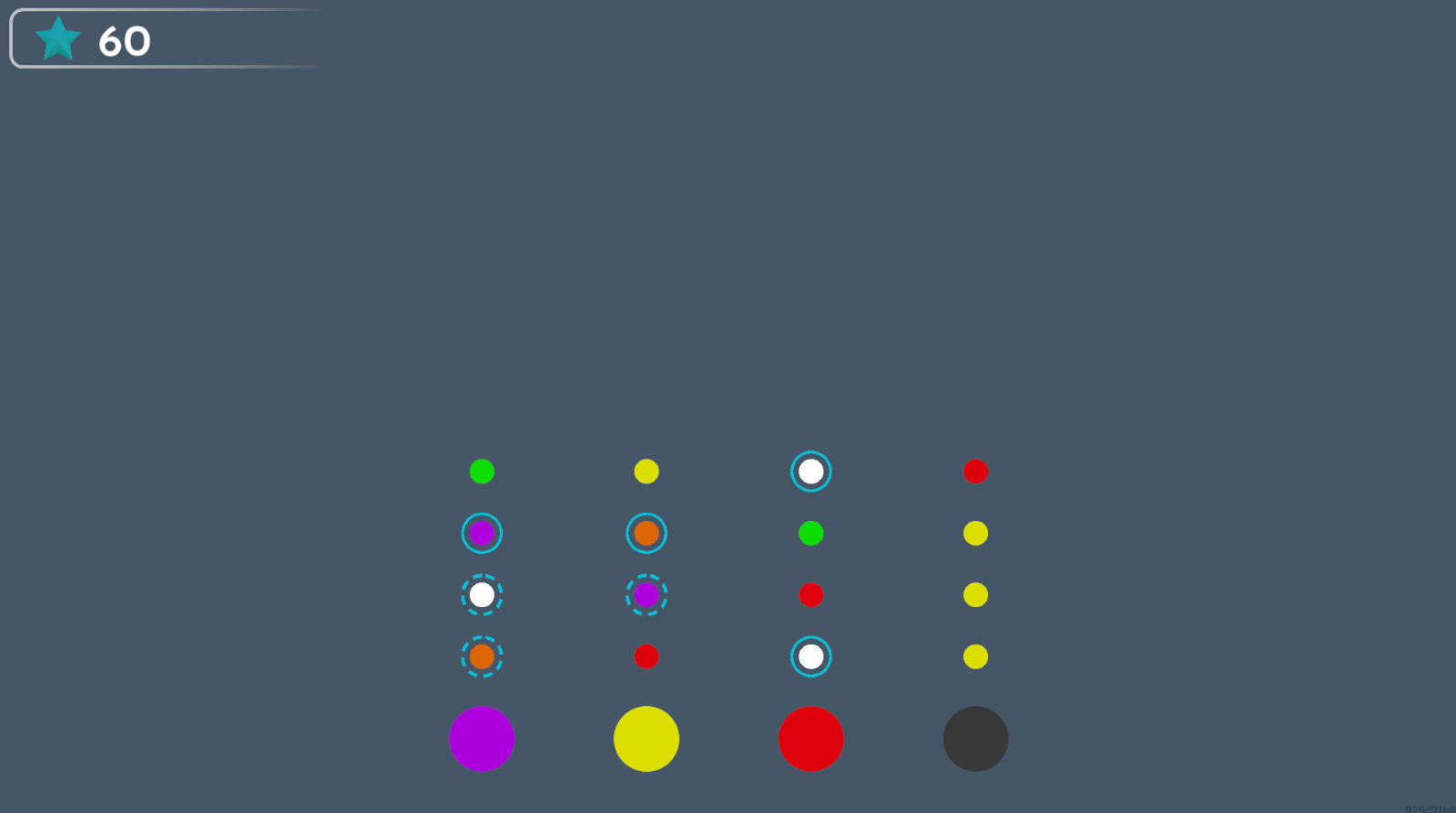
Large diversity of motor & cognitive exercises
Fine movements, attention, coordination
memory
visual exploration
executive functions
Visual representation, mental rotation
Coordination, attention, reactivity
Deduction, memory
Vicious circle of inactivity
Virtuous circle for recovery
Why set up a guided
self-rehabilitation lab?
1. Preventing the harmful effects of prolonged inactivity.
2. A rich environment based on cognitive and playful activities to stimulate
the patient and increase physical activity.
3. High level of clinical evidence on self-rehabilitation approach.
4. Ultra-intuitive and easy for all patients.
5. Intensive rehabilitation to encourage movement repetition.
6. Bimanual or unimanual motor training to constrain the use of the impaired limb.
7. Safe, seated or standing position.
8. Real-time adjustment of difficulty level according to patient recovery.
9. Performance monitoring
(activity time, number of movements, etc.).
10. Activities can be performed alone, with relatives or during group therapy session.
Discover
our other technologies

IVS
Intensive Visual Simulation